Other names: camp fever, jail fever, hospital fever, ship fever, petechial fever, epidemic louse-born typhus.
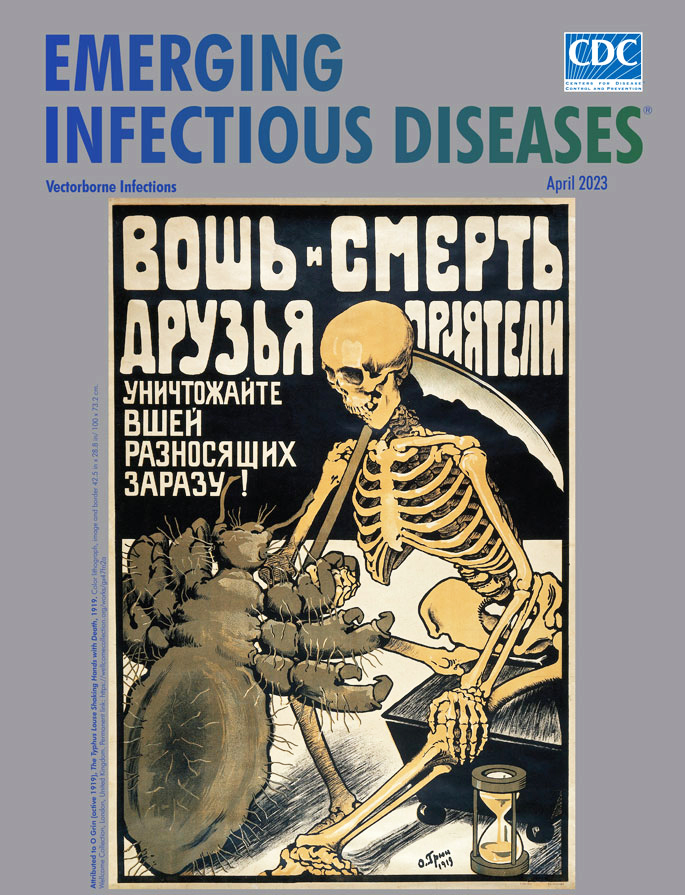
Epidemic typhus, also known as louse-borne typhus, is a form of typhus so named because the disease often causes epidemics following wars and natural disasters where civil life is disrupted.
Epidemic typhus is spread to people through contact with infected body lice, in contrast to endemic typhus which is usually transmitted by fleas.
Though typhus has been responsible for millions of deaths throughout history, it is still considered a rare disease that occurs mainly in populations that suffer unhygienic extreme overcrowding.
Typhus is most rare in industrialized countries. It occurs primarily in the colder, mountainous regions of central and east Africa, as well as Central and South America.
The causative organism is Rickettsia prowazekii, transmitted by the human body louse (Pediculus humanus corporis). Untreated typhus cases have a fatality rate of approximately 40%. Epidemic typhus should not be confused with murine typhus, which is more endemic to the United States, particularly Southern California and Texas. This form of typhus has similar symptoms but is caused by Rickettsia typhi, is less deadly, and has different vectors for transmission.
# Signs and symptoms
Symptoms of this disease typically begin within 2 weeks of contact with the causative organism. Signs/Symptoms may include.
- Fever
- Chills
- Headache
- Confusion
- Cough
- Rapid Breathing
- Body/Muscle Aches
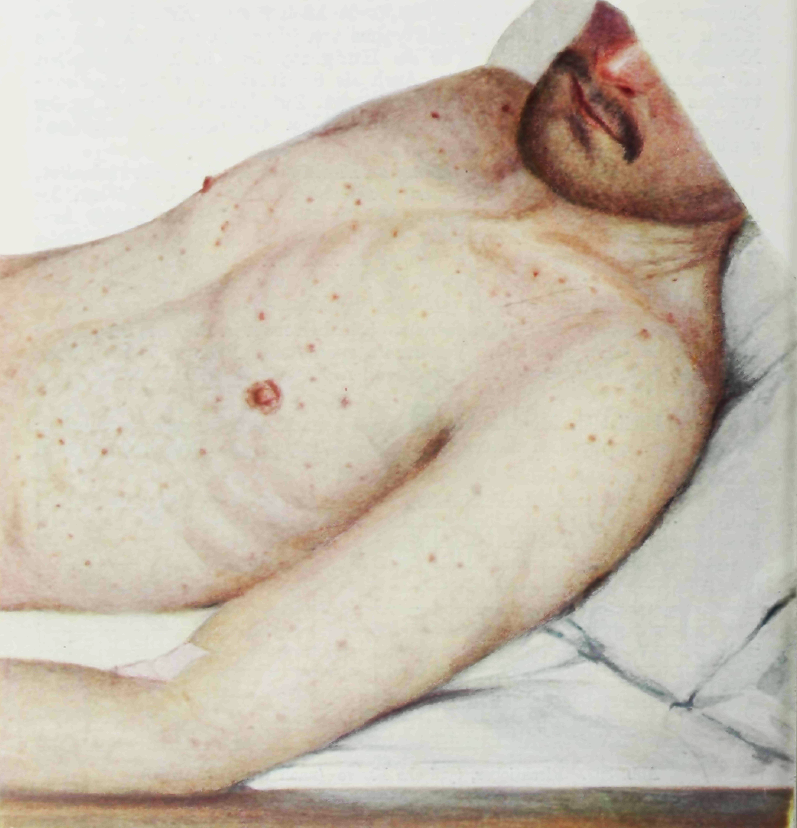
- Rash
- Nausea
- Vomiting
After 5–6 days, a macular skin eruption develops: first on the upper trunk and spreading to the rest of the body (rarely to the face, palms, or soles of the feet).
Brill–Zinsser disease, first described by Nathan Brill in 1913 at Mount Sinai Hospital in New York City, is a mild form of epidemic typhus that recurs in someone after a long period of latency (similar to the relationship between chickenpox and shingles). This recurrence often arises in times of relative immunosuppression, which is often in the context of a person suffering malnutrition or other illnesses.
In combination with poor sanitation and hygiene in times of social chaos and upheaval, which enable a greater density of lice, this reactivation is why typhus generates epidemics in such conditions.
# Complications
Complications are as follows
- Myocarditis
- Endocarditis
- Mycotic aneurysm
- Pneumonia
- Pancreatitis
- Kidney or bladder infections
- Acute renal failure
- Meningitis
- Encephalitis
- Myelitis
- Septic shock
# Transmission
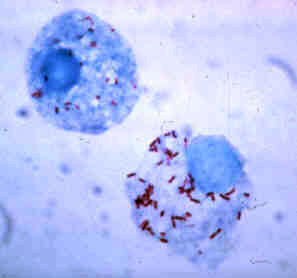
Feeding on a human who carries the bacterium infects the louse. R. prowazekii grows in the louse's gut and is excreted in its feces. The louse transmits the disease by biting an uninfected human, who scratches the louse bite (which itches) and rubs the feces into the wound.
The incubation period is one to two weeks.
R. prowazekii can remain viable and virulent in the dried louse feces for many days. Typhus will eventually kill the louse, though the disease will remain viable for many weeks in the dead louse. Epidemic typhus has historically occurred during times of war and deprivation.
For example, typhus killed millions of prisoners in German Nazi concentration camps during World War II.
The unhygenic conditions in camps such as Auschwitz, Theresienstadt, and Bergen-Belsen (Anne Frank died 1945) allowed diseases such as typhus to flourish.
Situations in the 20-first century with potential for a typhus epidemic would include refugee camps during a major famine or natural disaster. In the periods between outbreaks, when human to human transmission occurs less often, the flying squirrel serves as a zoonotic reservoir for the Rickettsia prowazekii bacterium. In 1916, Henrique da Rocha Lima proved that the bacterium Rickettsia prowazekii was the agent responsible for typhus; he named it after H. T. Ricketts and Stanislaus von Prowazek, two zoologists who had died from typhus while investigating epidemics. Once these crucial facts were recognized, Rudolf Weigl in 1930 was able to fashion a practical and effective vaccine production method.
He ground up the insides of infected lice that had been drinking blood. It was, however, very dangerous to produce, and carried a high likelihood of infection to those who were working on it. A safer mass-production-ready method using egg yolks was developed by Herald R. Cox in 1938.
This vaccine was widely available and used extensively by 1943.
# Diagnosis
IFA, ELISA or PCR positive after 10 days.
# Treatment
The infection is treated with antibiotics. Intravenous fluids and oxygen may be needed to stabilize the patient. There is a significant disparity between the untreated mortality and treated mortality rates: 10-60% untreated versus close to 0% treated with antibiotics within 8 days of initial infection. Tetracycline, chloramphenicol, and doxycycline are commonly used.
Some of the simplest methods of prevention and treatment focus on preventing infestation of body lice. Completely changing the clothing, washing the infested clothing in hot water, and in some cases also treating recently used bedsheets all help to prevent typhus by removing potentially infected lice.
Clothes left unworn and unwashed for 7 days also result in the death of both lice and their eggs, as they have no access to a human host.
Another form of lice prevention requires dusting infested clothing with a powder consisting of 10% DDT, 1% malathion, or 1% permethrin, which kill lice and their eggs.
Other preventive measures for individuals are to avoid unhygienic, extremely overcrowded areas where the causative organisms can jump from person to person.
In addition, they are warned to keep a distance from larger rodents that carry lice, such as rats, squirrels, or opossums.
Typhoid fever (Epidemic typhus)
Related
References
https://en.wikipedia.org/wiki/Epidemic_typhus Photo
wikipedia
CDC
- Actinomycosis
- Anthrax
- Biopsy Sinusitis_Aspergillus flavus
- Botulism
- Brucellosis
- Cat Scratch Disease
- Cellulitis
- Cholera
- Creutzfeldt-Jakob Disease
- Cystic Fibrosis_CF
- Diphtheria
- Erysipelas
- Erysipeloid or fish poison
- Legionnaires disease
- Lemierre syndrome
- Leprosy
- Listeriosis
- Lyme / Borreliosis
- Melioidosis
- Meningitis
- Plague
- Syphilis
- Tetanus
- Trench Mouth_Plaut-Vincent_acute necrotizing ulcerative gingivitis
- Tuberculosis (TB)
- Tularemia_Rabbit Fever
- Typhoid fever (Epidemic typhus)
- Whooping Cough