Heroin for a little cough, worm eggs for overweight, and mummy powder for stomach ulcers. Doctors and quacks alike shunned no remedy in their attempts to cure the patient.
♦ Heroin helped with coughing
German cold sufferers—adults and children alike—were the first to be prescribed the new miracle drug: heroin. Manufacturers made millions.
When heroin came onto the market in 1898, it was, according to the German pharmaceutical company Bayer, an effective and inexpensive remedy for coughing, colds, and pain. It was also said to help the many people who had become addicted to the painkiller morphine overcome their dependency.
In Bayer’s laboratories, a team of chemists led by Heinrich Dreser had discovered in 1895 that the substance diacetylmorphine was a better and stronger painkiller than morphine.
The miracle drug was called ‘heroin,’ from the Greek word heros (hero), because users reportedly felt brave and vigorous after taking it. The substance was used, among other things, to treat bronchitis and in children with persistent coughs
The drug caught on quickly, especially in the United States, and the Bayer company made a fortune. But patients began to complain about addiction. Inside the body, diacetylmorphine was found to be converted into morphine. In 1914 the use of heroin in the U.S. was restricted, and in 1925 it was banned as a medicinal drug.
Effect: Diacetylmorphine is analgesic but highly addictive when used regularly. An overdose can be fatal.
♦ Fluid drained from inflamed lungs
Pneumonia can lead to a buildup of fluid in the lungs. This makes breathing difficult, and without treatment, patients can die from it.
The father of medicine, the Greek Hippocrates, therefore devised a way to drain fluid from the lungs by cutting open the chest.
More than 2,000 years later, European and American doctors drew inspiration from Hippocrates when searching for a remedy for the flu, which had killed 50 to 100 million people worldwide in 1917 and 1918.
During World War I, the disease spread rapidly on American military bases, and doctors needed a method to quickly remove fluid from the lungs of flu patients. To do this, they simply removed the ribs that were in the way.
Effect: The lungs were drained, but most patients died from a collapsed lung.
♦ Trepanation (skull drilling) cured the insane
Since the early Neolithic period, from around 3000 BC, people have been making holes in the skull. This was done to drive out bad blood and evil spirits.
In the Hippocratic treatise On Head Wounds from 400 BC, trepanation, or skull drilling, is recommended for patients who had injured their heads.
According to the ancient Greeks, a blow to the head could cause accumulations of blood, which would develop into pus and could be removed by making a hole with a trepan, a small drill.
In China, headaches were treated with skull drilling during the Han dynasty (168–280 AD), and from the Middle Ages to the 19th century, the mentally ill and epileptics were subjected to this treatment because it was believed that stones or air were trapped in their heads.
Only 10 percent of patients survived the procedure; many died from infection. Trepanation still occurs among some African tribes, and there are also practitioners in the West, such as the American Peter Halvorsen, who treated his depression with skull drilling in 1972
Effect: If the brain is under pressure, trepanation can sometimes be useful, but it does not help with conditions such as depression
♦ Brain incisions
In the 20th century, psychosurgery emerged, with lobotomy becoming particularly popular.
Patients with psychosis faced the risk of being sedated with electric shocks and having a probe inserted into the brain through the eye.
By moving the probe up and down, the doctor severed the nerves leading to the frontal lobe, which governs behavior
The method was developed in the 1930s by the Portuguese doctor Egas Moniz, who won the Nobel Prize in Physiology or Medicine in 1949. On January 17, 1946, the American doctor Walter Freeman ‘refined’ the procedure.
He took an ice pick from his kitchen and drove it through the eye of 29-year-old patient Ellen Ionesco.
Before the operation, she was suicidal, but afterwards she was able to leave the institution and return to live with her family. Freeman called his method the transorbital lobotomy, or ice pick lobotomy.
By 1957, Freeman had operated on 2,400 patients, and worldwide tens of thousands of people underwent lobotomy in the 1950s and 1960s—including 40,000 in the U.S. and 17,000 in the U.K.
In 1950, the drug chlorpromazine was introduced, known as the chemical lobotomy, and in the following years the surgical procedure was largely replaced by psychopharmaceuticals
Effect: Lobotomy relieved anxiety, but left many patients apathetic and disoriented, and caused memory loss and epilepsy
♦ Treatment of hemorrhoids with red-hot iron
The ancient Greeks mentioned red-hot iron as a possible treatment for hemorrhoids as early as 400 BC. A heated iron rod was inserted into the anus, and the patient was advised to scream loudly so that the bowel would expand, giving the doctor better access.
Over 1,000 years later, the Irish monk Fiacrius devised a slightly more humane method. He discovered that sitting on a warm stone eased his hemorrhoids.
Patients flocked to him, and after his death in 670, he was canonized. Hemorrhoids became known as ‘the curse of Saint Fiacrius.’
Meanwhile, the glowing iron rod had come back into use, and hemorrhoids are still sometimes cauterized under anesthesia
Effect: Red-hot iron can cause burns and infections.
♦ Electric shocks for impotence
When customers of the American department store Sears, Roebuck & Co. browsed the catalog in 1900, their eyes fell on a new, modern device: the Heidelberg Electric Belt.
The belt produced a ‘constant, soothing alternating current that strengthens weak points, builds systems, and promotes circulation.’ Anyone who wore the device around their genitals and waist was said to be cured of almost everything: fatigue, gout, sciatica, back pain, insomnia, kidney and liver disorders, and a weak heart. The Heidelberg Belt also helped with ‘female weakness,’ and in men impotence was treated ‘by restoring strength after the harmful effects of masturbation.’
The Heidelberg Electric Belt was not the only device of its kind. From 1892, London women who could afford it could purchase an electric corset, and The Electric Belt Company and Addison’s Galvanic Electric Belt profited from the curiosity surrounding modern electricity
Effect: Electrical impulses can relieve pain and help rebuild muscle mass after spinal cord injury, but there is no evidence that they cure impotence
♦ Orgasm was used to treat female hysteria
Since ancient times, it has been believed that many women suffer from ‘hysteria,’ a chronic condition that makes them difficult to manage.
In the 2nd century, the Greek physician Galenus stated that hysteria in women was caused by sexual abstinence.
In the 10th century, the Persian physician and philosopher Avicenna suggested a ‘massage treatment,’ which would bring ‘relief’ to afflicted women. Using some oil on his fingers, he massaged the vagina, producing the relieving ‘paroxysm’—an orgasm.
Because this treatment was time-consuming and left the physician with a sore hand, many practitioners welcomed the arrival of the electric vibrator in the 1880s. The British doctor Joseph Mortimer Granville patented the invention. It was widely known and accepted that women could derive sexual pleasure from the male genitalia—so it was not considered unethical for doctors to ‘lend a hand’ on the treatment table.
The Vibratile was sold widely until the 1920s, when the vibrator began to be regarded as improper
Effect: The diagnosis of ‘hysteria’ has not been made since the 1950s, and the vibrator is no longer considered a medical instrument
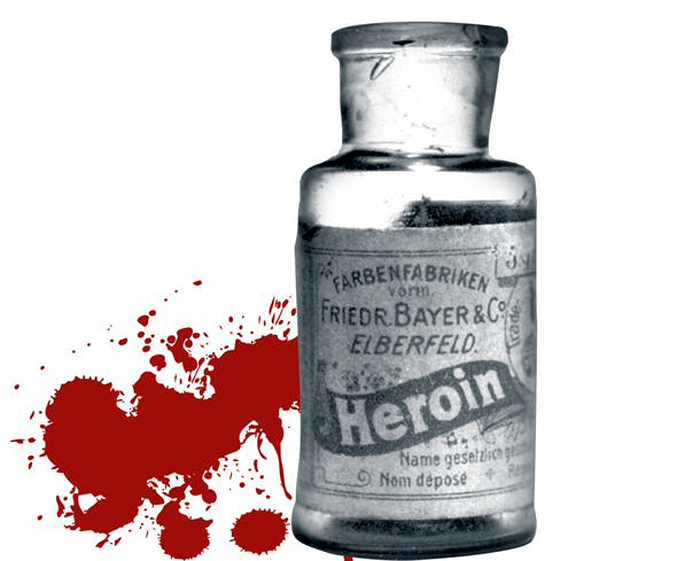
♦ TB patients were treated by inserting pellets into their lungs
In the 19th and 20th centuries, tuberculosis was a major cause of death.
Physicians were urgently seeking a cure, and when the Italian doctor Carlo Forlanini discovered in the 1880s that the constant movement of the lungs during breathing hindered the healing process, the next step was quickly taken: the affected part of the lung needed rest.
This was achieved by creating an artificial pneumothorax in the diseased area. This allowed the organ to rest and heal. There were several methods to induce a pneumothorax. In a widely used treatment, part of the lung was filled with plastic pellets, which caused the area to collapse.
From the 1940s and 1950s, tuberculosis could be treated with medication, and the artificial pneumothorax was no longer used.
Usually, the pellets were not removed after the procedure, and sometimes, to the surprise of doctors, they appeared on an X-ray up to 40 years later.
Effect: The treatment was often successful, but unfortunately the side effects were severe. Many patients developed lung infections or cancer.
Source: Historia
Doctors’ advice did more harm than good
References
Historia
Photoos
Wikipedia
© Corbis/Polfoto/Bayer AG_heroin
© Wellcome Library, London
© SSPL/Polfoto/Brooke Clarke

Art lijst
Schilderijen
- Bosch, Hieronymus – The Peddler
- Bosch, Hieronymus_The Haywain triptych
- Botticelli, Sandro_Primavera / Spring
- Brueghel the Elder, Pieter – The Tower of Babel
- Campin, Robert — Mérode Triptych
- Courbet, Gustave_The painters Studio
- Dali, Salvadore_The Temptation of Saint Anthony
- Dou, Gerard_the Quack Doctor
- Eyck van Barthélemy_Still life with books
- Fra Angelico_Annunciation
- Géricault, Théodore_Medusa's raft
- Magritte, Rene_Prohibited to depict
- Matsys, Quinten_The money changer and his wife
- Memling, Hans_Twee paarden in een landschap
- Onbekend-16e eeuw_4 gedaantes van een arts
- Picasso, Pablo_Guernica
- Rembrandt_Abraham en de drie engelen
- Rembrandt_Elsje Christiaens
- Velazquez, Diego_Las Meninas
Schilderijen en de dokter
- Agenesia Sacrale (a rare congenital disorder in which the fetal development of the lower spine)
- Alopecia areata (hair loss)
- Arthrogryposis congenita (birth defect, joints contracted)
- Artritis psoriatica (inflammatory disease of the joint)
- Artritis reumatoïde
- Breast development (delayed)
- Bubonic plague
- Diphtheria
- Gigantism and Acromegaly
- Goiter (struma)
- Hare lip (cheiloschisis) / cleft palate
- Herpes zoster (shingles)
- Hunger edema
- Influenza Epidemic of 1858
- Insanity - Malle Babbe (1640)
- Leprosy
- Lovesick, pregnancy
- Lymph node tumor (lymphoma), non-Hodgkin
- Manic Depression Psychosis
- Measles / Rubella? (acute viral infection)
- Melanoom of naevus (geboortevlek)
- Membraneuze glomerulonefritis
- Moord (pneumothorax, slagaderlijke bloeding)
- Neurofibromatose
- Oogoperatie
- Osteoartrose / hallux valgus
- Osteomyelitis
- Otitis media (acute middenoorontsteking)
- Parotitis (mumps)
- Platvoet en Spitsvoet
- Polio
- Prepatellaire bursitis
- Progeria
- Pseudohermafroditisme
- Pseudozwangerschap
- Psychoneurose (acute)
- Rachitische borst
- Reumatische koorts (acute)
- Rhinophyma of knobbelneus
- Rhinophyma rosacea_depressie
- Rhinoscleroma
- Schimmelziekte_Favus
- Syfilis (harde 'sjanker')
- Tandcariërs
- The Extraction of the Stone of Madness
- Tuberculose long
- Ziekte van Paget
Schilders
Historie lijst
- 1632-1723_Antonie van Leeuwenhoek
- 1749-1823_Edward Jenner
- 1818-1865_Ignaz Semmelweis
- 1822-1895_Louis Pasteur
Wetenswaardigheden lijst
- 1887 Psychiatric Hospital
- Animals on duty
- Bizarre advice for parents
- Bloodletting
- Bloodthirsty Hungarian Countess Elizabeth Báthory (1560–1614)
- Butler escaped punishment three times.
- Dance mania / Saint Vitus Dance
- Doctors’ advice did more harm than good
- French Revolution Louis XVI
- Frontal syndrome (Phineas Gage)
- Heart disease (Egyptian princess)
- Ice Age (minor)_1300-1850
- Ivan IV de Verschrikkelijke (1530-1584)
- Kindermishandeling
- Koketteren met koningin Victoria
- Koningin door huidcrème vergiftigd
- Kraambedpsychose (Margery Kempe)
- Massacre in Beirut
- ME stonden bol van de seks
- Mummie bij de dokter
- Plee, Gemak of Kakstoel
- Prostaatkanker (mummie)
- Sexhandel in Londen
- Swaddling baby
- Syfilis was in de mode
- Testikels opofferen
- Tropische ziekten werden veroveraars fataal
- Vrouwen als beul in WOII
- Wie mooi wil zijn moet pijn lijden
- Zonnekoning woonde in een zwijnenstal

.jpg)



.jpg)